Hospitalizations account for nearly one-third of the total $2 trillion spent on health care in the United States, according to the Institute for Healthcare Improvement. Though most hospitalizations are necessary, too often patients are re-admitted soon after their initial hospital stay. Such readmissions are both costly and often avoidable.
Holton Community Hospital (HCH) in northeast Kansas achieved a 46% improvement in their Unplanned All Cause 30-Day Readmissions Rate between September 2020 and February 28, 2022. Through their work with HQIC and the KHC, they implemented a unique Readmission Risk Assessment and developed a proactive approach to care coordination, which resulted in the dramatic improvement of the hospital’s readmission rate.
 HCH Quality Director Cody UtzIn 2012, hospital leadership sent their Quality Director and one nurse to the KHC’s annual Summit on Quality. They attended a learning session on readmissions and returned to Holton motivated to begin improvement work on readmissions with the idea of hiring a Patient Care Coordinator.
HCH Quality Director Cody UtzIn 2012, hospital leadership sent their Quality Director and one nurse to the KHC’s annual Summit on Quality. They attended a learning session on readmissions and returned to Holton motivated to begin improvement work on readmissions with the idea of hiring a Patient Care Coordinator.
They created a multifunctional Care Transitions Team, which has evolved over the years to include medical staff providers, hospital and primary care clinic staff, hospital leadership team members, pharmacy, home health, hospice, rehabilitation, and social workers. Ten years later, the Care Transitions Team remains at the center of their effort to prevent avoidable readmissions and hospitalizations, as well as promote appropriate use of the Emergency Department.
Prior to 2019, HCH was able to achieve and maintain an All Cause 30-Day Readmissions rate averaging about 3% for Unplanned All Cause 30-Day Readmissions. They were content with their performance and shifted focus to other quality improvement priorities. In September 2020, HCH enrolled in the Compass Hospital Quality Improvement Contract (HQIC) initiative, which is funded by CMS. Cody Utz, Director Patient Care Services and Quality, worked with the Kansas Healthcare Collaborative to select priorities for their Quality Improvement Work Plan, which identified Care Transitions and Readmission Reduction as one of their top three priorities for improvement. They reviewed their baseline data for readmissions from 2019 which revealed their Unplanned All-Cause 30-Day Readmissions rate reached 7.23% by December 2019, revealing both a challenge and opportunity for improvement.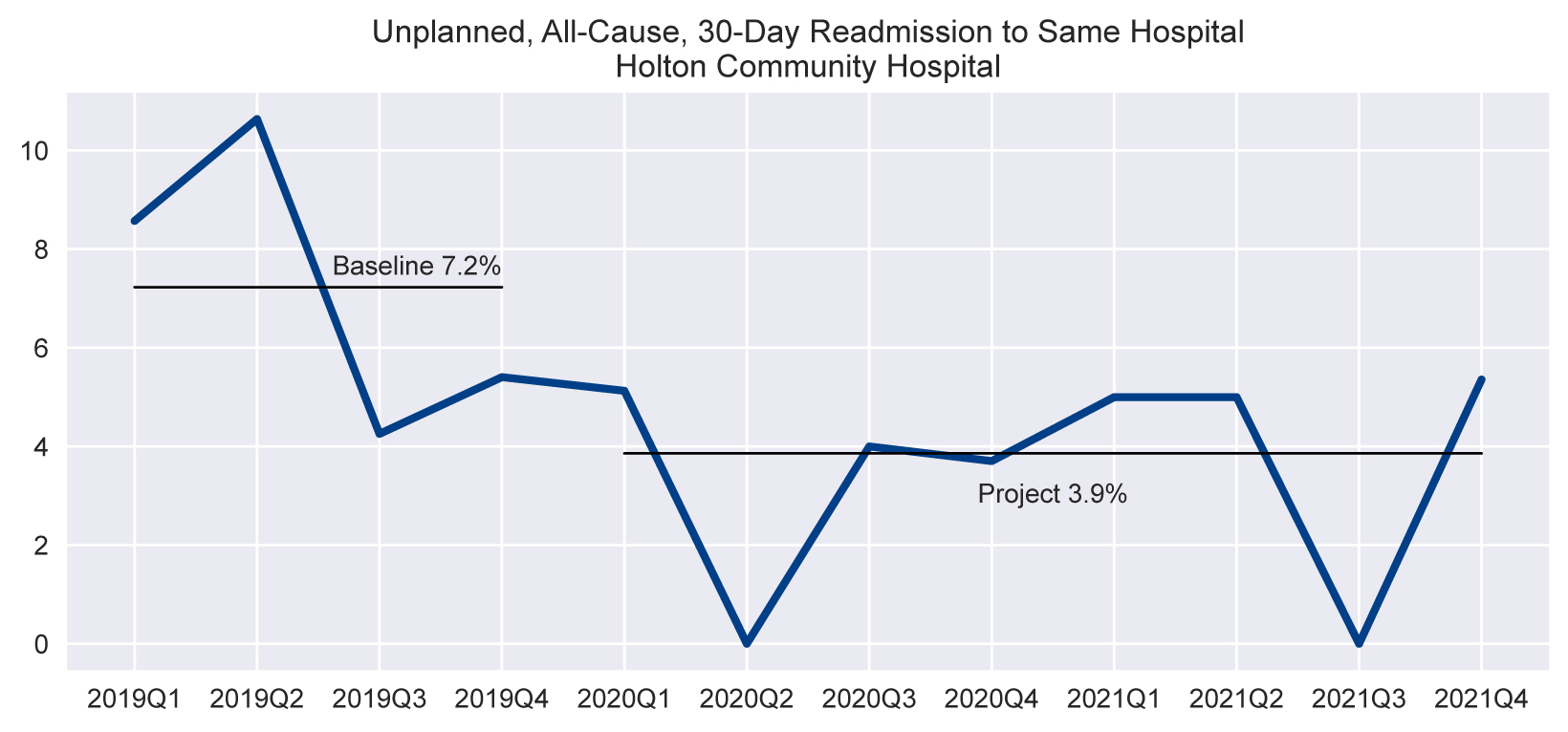
The hospital’s initial readmissions project focus in 2021 was to revise the current readmissions risk tool and procedures for its use in the hospital, Utz said. They set a readmissions goal for 2021 to achieve and sustain a rate of 3.2% or lower for Unplanned All Cause Readmissions. Their interventions to achieve the goal started with reviewing both the LACE and PLACES tools. Staff members liked elements from both tools and therefore chose to create a unique hybrid readmissions risk assessment tool, which includes key elements from both tools. It is now the foundation for HCH’s readmission improvement.
Patient Care Coordinators administer the risk assessment upon admission, which then guides care during the hospital stay, discharge planning, and Transitional Care Management post-discharge. After patients are discharged, Patient Care Coordinators provide patient outreach within the first two days at home and again generally around one-week post-discharge. The Patient Care Coordinators identify unmet needs, barriers to care, medication adherence, understanding of discharge instructions, and care plans as well as answering patient and family questions. They solicit honest feedback regarding the patient’s hospital stay and share feedback — both positive and negative — with providers and staff. ‘Thank You’ cards are created when patients want to share positive feedback on their hospital stay and often recognize individual staff for excellent patient care. These cards have been highly motivating for staff, particularly during a year where the pandemic resulted in pervasive staffing challenges and fatigue.
Information from patient outreach encounters is shared with the primary care provider as well as during the Transition of Care meetings. It includes outreach statistics, interventions provided, and any systems issues that might have been identified during this process. Readmissions data is shared quarterly with providers and staff, including Medical Staff Meetings, HCH’s staff newsletter, Board of Directors meetings, and on the hospital’s public Quality Board, which is located in a high traffic area of the facility. HCH Care Coordination Team (L to R) Sandy Jones, RN, Patient Care Coordinator; Breann Hinman, RN, Patient Care Coordinator; Leigh Ann Schultejans, LMSW, Director of Care Coordination.
HCH Care Coordination Team (L to R) Sandy Jones, RN, Patient Care Coordinator; Breann Hinman, RN, Patient Care Coordinator; Leigh Ann Schultejans, LMSW, Director of Care Coordination.
When asked what advice she would offer facilities who wish to embark on an improvement project for readmissions, Utz said: “You need to celebrate that success, because that is amazing work!” She says the adage “it takes a village” certainly applies to reducing readmissions. She recommends starting with small tests of change. Identify one key intervention that you feel will result in the biggest impact in your organization and work to create “hard-wired” processes.
Utz advises hospitals to not take on too many changes at once or staff may feel overwhelmed and may be more likely to give up on their efforts. Through this decade of readmissions work, they have identified some key learning points. The hospital’s dedication to preventing readmissions and focusing on transitions of care has been a “huge benefit” to primary care providers. She said having the provider’s prospective and knowledge on the Transitions of Care Team has been integral to the team’s success.
HCH will readily attest that a successful readmissions program never ends. To achieve goals and maintain improvement, the work is by necessity ongoing. Though the hospital narrowly missed its 2021 goal of achieving a 3.2% or better Unplanned All Cause 30-Day Readmission rate, they were able to achieve a rate of 3.8%. Through the work of the Transitions of Care Team and having providers review clinical cases, HCH has identified a correlation between patients who have chronic conditions and a behavioral health diagnosis who are seeking care in the Emergency Department and who are readmitted.
In conjunction with the Kansas Healthcare Collaborative, KHIN and COPIC, Holton Community Hospital is participating in the “Align All Health” initiative which is a targeted intervention for hospitals and community mental health centers to improve health outcomes and care transitions for high-risk behavioral health patients. In addition to implementation and training to use the KHIN Dashboards and acute alerts for high-risk patients, participating facilities implement procedures to identify attributable behavioral health patients to monitor care transitions for high-risk patients.
For more information about the Align All Health Program, visit www.alignallhealth.org or visit KHC’s website www.khconline.org for information about other quality improvement initiatives.
