 Some of the more than 700 team members at Labette Health.
Some of the more than 700 team members at Labette Health.
Quality improvement goal: Our goal was to reduce avoidable readmissions to as near to zero as possible.
We started in partnership with the Kansas Healthcare Collaborative in 2012 through the Hospital Engagement Network (HEN) 1.0, HEN 2.0, and the current Hospital Improvement Innovation Network (HIIN). Since then, we have grown in how we approach and monitor performance improvement projects. Early on, this institution felt that readmissions reduction was a quality department-driven objective — but over the course of this and other projects, we have seen a culture change in institution. Directors and front-line staff see the quality department as a tool and as support for accomplishing ambitious goals.

Labette Health is a 99-bed hospital in Parsons, a community of 11,500 residents in southeast Kansas. It provides acute, intensive, and inpatient rehabilitation services. |
Interventions selected were what felt natural to the flow of the organization, as well as alterations to current processes. The most fundamental intervention that is now at the core of all Labette Health’s processes is transparency of data.
Making sure all key players are at the table has been crucial. Our team has maintained a multidisciplinary approach including case managers, the chief nursing officer, quality department, respiratory therapy, front-line staff, and providers.
And of course, the dedicated efforts of our team members have been critical to our success in reducing readmissions. The biggest driver for reducing preventable readmissions has been case managers, as they were the ones talking to patients and tracking the information. They include: Traci Journot, RN; Linda Clarenson, RN; Mark Knight, RN; and Angie Rankins, RN. Admission Nurse Jennifer Babb, RN, was essential in identifying the patients’ comments on why they were being readmitted and directing questions in the initial interview. In the beginning the initiative was led by Tereasa DeMeritt, (APRN, Quality Director) as she participated in KHC Quality Improvement Fellowship program. Another key player in understanding our readmission population was Rachel Merrick, RN, as she was able to utilize excel charts to analyze the data to find our key areas of concern and trends over the years.
How was the data collected and used to guide your process improvement efforts?
 To gather data, case managers would keep a spreadsheet log of all inpatient and observation patients that were readmitted within 30 days. Using this information, the quality department would analyze the data to reveal trends and opportunities. In 2012, we had an average of 18 total readmissions monthly, so it was important to focus on readmission as a whole, not just individual specialties.
To gather data, case managers would keep a spreadsheet log of all inpatient and observation patients that were readmitted within 30 days. Using this information, the quality department would analyze the data to reveal trends and opportunities. In 2012, we had an average of 18 total readmissions monthly, so it was important to focus on readmission as a whole, not just individual specialties.
Describe the results including patient outcomes, process changes, and service delivery results.
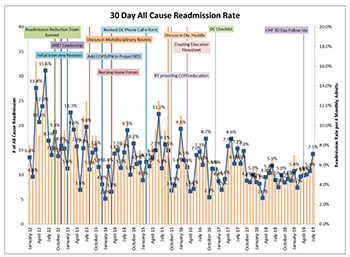
Our improvement initiative started with an overall awareness of the issue by gathering information and our baseline data. In 2012, our annual readmission rate was 9.2%. By the end of 2014, we reduced our readmissions rate to 6.1%, a reduction of 33%.
In 2015, we revised the discharge phone call e-forms to aid the caller in more specific questions, started recognizing readmission in the morning daily huddles, and respiratory staff started providing more comprehensive COPD patient education. These interventions did not show any immediate decrease but contributed to improvement in 2016, which had a major change in modifying a discharge planning checklist that case managers use when speaking to patients. That year showed a 35.5% decrease since the 2012 baseline.
For the following years, we continued to work and refine our processes. We achieved a 51.6% reduction in 2018 compared to the original 2012 baseline. During the current HIIN initiative we had noticed a slight increase in readmissions among our heart failure patients, so case managers implemented a 30-day follow-up process for that population. Currently, we have seen a 23.2% reduction in the HIIN program (Oct. 2016 to July 2019) for overall 30-day readmissions.
To date, our annual 2019 rate is 43.2% lower than our 2012 overall baseline.
 Labette Health team members include (from left) Emily O’Brien, RN; Tereasa DeMeritt, APRN; Sarah Vaughan, RN; and Rachel Merrick, RN.Lessons Learned
Labette Health team members include (from left) Emily O’Brien, RN; Tereasa DeMeritt, APRN; Sarah Vaughan, RN; and Rachel Merrick, RN.Lessons Learned
Transparency has been the primary key to our successes and helps promote effective communication and coordination of care. When it comes to reducing avoidable readmissions, transparency promotes much more effective discharge planning and morning huddles.
Next Steps
Readmissions will always be an area of process improvement for Labette Health. We understand zero is not a realistic or achievable goal in all-cause 30-day readmissions, but nevertheless we continue to strive to lower readmissions rates.
In the last few years with the increased awareness of sepsis and early identification, we have seen an increase in sepsis readmissions or diagnosis of such. Future plans include a further dive into why sepsis patients are being readmitted by interview processes and analyzing the data. Education for staff on the risk of sepsis and the increase likelihood of readmissions in this population will be provided. We also plan to engage the community in a variety of ways about the dangers and symptoms of sepsis.
Labette Health Readmissions Toolkit
