Osborne County Memorial Hospital team members (from left) include Cindy Hyde, Risk Manager; Kristen Hadley, Quality Improvement Coordinator; Lori Rothenberger, RN and Assistant Director of Nursing; and Monica Mullender, RN and Director of Nursing.
Osborne County Memorial Hospital team members (from left) include Cindy Hyde, Risk Manager; Kristen Hadley, Quality Improvement Coordinator; Lori Rothenberger, RN and Assistant Director of Nursing; and Monica Mullender, RN and Director of Nursing.
Quality Improvement Goal: Reduce patient falls with injury by 30% or more from 2018 to 2019.
The quality improvement team at Osborne County Memorial Hospital (OCMH) is led by Quality Improvement Coordinator Kristen Hadley. By participating in the statewide Hospital Improvement Innovation Network (HIIN) led by the Kansas Healthcare Collaborative (KHC), Hadley and her team have access to comparative data reports that help inform and guide the hospital’s quality improvement efforts.
“Our data reports indicated that we were coming in higher than the state average for falls,” Hadley said. “Leadership was on board from the beginning when we made a commitment and priority to preventing falls with injury.”

|
Addressing the Challenge: Project Design
OCMH joined the KHC Falls Sprint initiative—a quality improvement collaborative anchored by monthly webinars, goal setting, action plans, and testing changes—conducted from October 2018 through March 2019. This statewide learning community worked together with KHC and national faculty, Cynosure Health, to identify opportunities for improvement and apply targeted strategies involving patients and families in fall prevention.
The hospital established an internal team to lead its fall prevention initiative, including Hadley; Cindy Hyde, risk manager; Monica Mullender, director of nursing; Lori Rothenberger, assistant director of nursing; and Aaron Geist, physical therapy.
In 2018, the hospital had 11 falls on the nursing floor. The team established a goal for 2019 to reduce the number of falls on the nursing floor by 30%.
Improvement Strategies
Through the KHC Falls Sprint, the hospital conducted an assessment of current practices and identified opportunities for improvement. The hospital tested:
- increasing fall risk assessments to every 12 hours, rather than 24 hours;
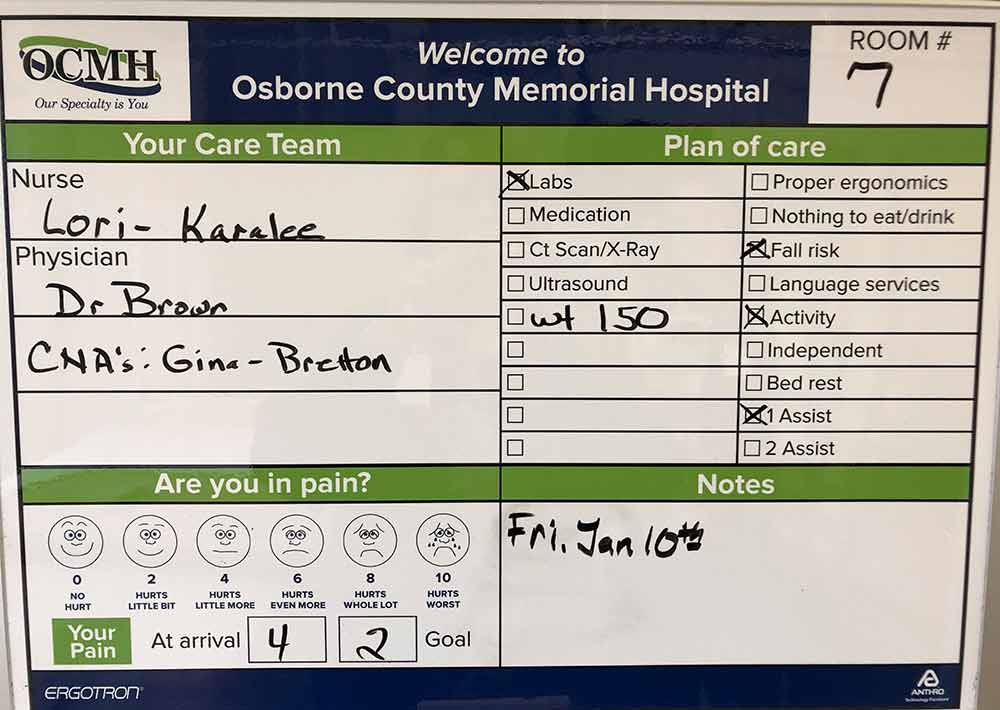
- more frequent rounding and utilizing white boards in patient rooms; and
- a new falls huddle process—which would include the patient and caregivers whenever possible—within 15 minutes of the patient fall to evaluate factors leading to the fall and to learn how subsequent falls could be prevented.
The improvement team provided education to staff about the hospital-wide fall prevention initiative, changes that were being tested, and enlisted their engagement. Front-line nurses began more frequent, purposeful rounding; conducting the Morse Fall Risk Assessment on every 12-hour shift; and listing the ambulatory status on the patient white boards. Hadley noted that their electronic health records now have a “hard stop” requiring fall assessments every 12 hours.
(story continues below video)
| Cindy Hyde, Risk Manager (left) and Kristen Hadley, Quality Improvement Coordinator, discuss the use of white boards and patient engagement in their hospital’s fall prevention initiative. |
Patients at elevated risk for falls are identified with a “falling star” signing on the outside of their door. The status also is added to the white boards.
“We found that no one was using the white boards,” said Hadley. “With education and coaching, nurses began using them with bedside rounding and including mobility status for staff, patients, and family to see.”
The hospital credits the education and tools shared through KHC’s Falls Sprint in providing resources to support their efforts.
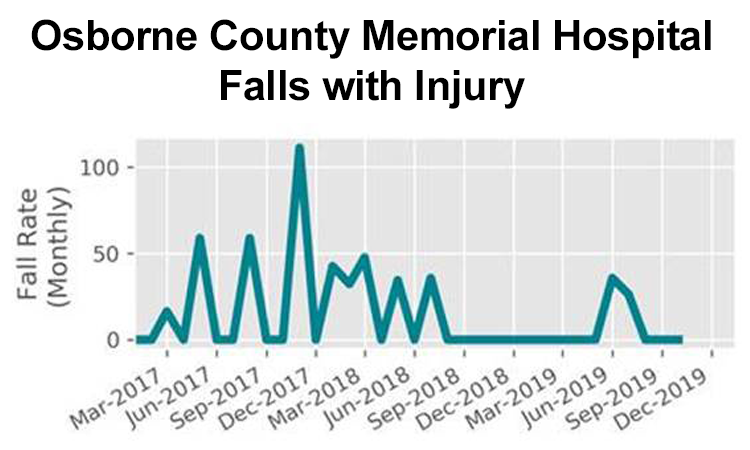
By utilizing the run chart provided by KHC in the data analytic report for falls, the hospital was able to see its monthly results over time. The Osborne quality improvement team also shared these monthly outcomes with front line staff and hospital leadership.
Hospital staff have found that it is beneficial to involve the patients and families in fall prevention efforts. Their post-fall huddles now involve the patients and family whenever possible, as they often have valuable insight as to identifying contributing factors in the fall.
During the hospital’s bi-monthly nurses’ meetings, staff are taught methods for enlisting the help of patients and families during the post-fall huddle, such as “What do you think happened?” And “How could we keep this from happening again?”
Often the patients themselves have the best ideas about ways they can prevent future falls, said Hadley. “Their engagement leads to more positive outcomes,” she said.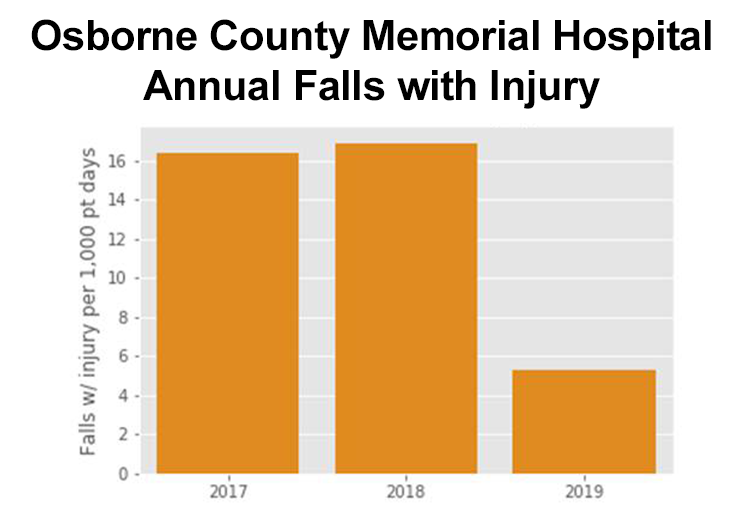
Upon discharge, a falls flyer is provided to patients to take home. Also, patients receive a follow-up phone call by the hospital’s social services designee.
The hospital’s culture and expectations around falls has dramatically changed for the better, Hadley said. In the past, staff may have assumed that falls were “just going to happen,” and now, the culture is, “We can make a difference.”
Lessons Learned
Through this initiative, the Osborne County quality improvement team found that leadership and staff engagement and empowerment were crucial. They also found engagement of patient and family led to more positive outcomes. In addition, through more frequent rounding, nurses were able to identify clinical changes in patients’ health earlier, which were beneficial to patient care.
The three most important drivers that produced the desired results were:
- Increasing frequency in fall risk assessments,
- Utilizing post-fall huddles, and
- Performing more frequent rounding with patients.
Hadley said that hospitals implementing a falls prevention program should start small and recognize it will take time for changes to become incorporated into routine care.
|
Toolkit Reducing Patient Falls at Osborne County Memorial Hospital |
Spread and Sustainability
The hospital began to see noticeable improvement soon after it implemented its program. The hospital plans to continue into 2020 its three key strategies adopted last year during the KHC Falls Sprint. The hospital has also begun posting how long since the last patient fall occurred.
Hadley said her team would continue to adopt other promising practices. Currently, her team is preparing fall prevention information for inclusion in the admission packet for patients and families. The team plans to develop a system for routinely sharing data and results with leadership and staff. They also plan to improve ambulation and usage of gait belts, with training and assistance from physical therapy. Looking ahead, the coming new hospital will feature overhead lifts to aid staff in mobilizing patients.
Hadley said one key theme from the KHC Falls Sprint that has been embraced by staff is: “If the patient comes in walking, they need to go out walking.”
“It would be exciting for our staff to see the results of their fall reduction efforts as we are committed to improving our outcomes and patient safety,” said Hadley. “They are involved, and with front-line staff ownership, we are identifying unsafe conditions—such as slippery socks—and continue to brainstorm different ways to help prevent falls.”